Palate Procedures & Treatments for Snoring & Sleep Apnea
Here at Indigo ENT, we work with a multidisciplinary team including respiratory therapists, sleep dentists, weight loss specialists, sleep therapeutic companies, respirologists and cardiologists.
Diagnosis of sleep apnea is provided typically on site through home sleep evaluations, scored and interpreted by our accredited sleep physicians.
Treatment typically involves a diet, weight loss and exercise program as an adjuvant to non-invasive therapies such as CPAP (continuous positive airway pressure), mandibular advancement devices and lastly, surgical intervention.
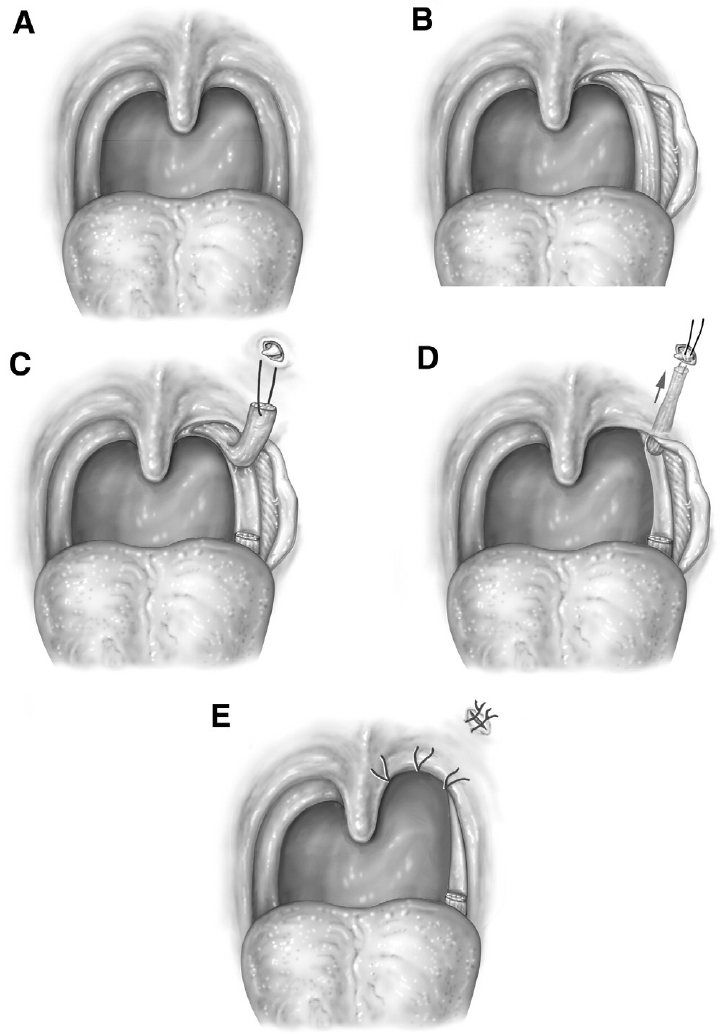
Surgery is customized to every individual patient. Indigo ENT provides a range of surgical procedures to treat snoring and obstructive sleep apnea, tailoring treatments to fit your needs. We focus on finding the best results with the lowest risks.
Nasal Surgeries & Procedures
One major contributor to snoring and obstructive sleep apnea is nasal obstruction. Various nasal treatments exist from non-surgical like medication and external nasal dilators (i.e. Breathe-right strips) to surgical procedures like rhinoplasty and nasal valve surgery, septoplasty, sinus surgery, and turbinate surgery. For more information go to Nasal Surgeries & Procedures.

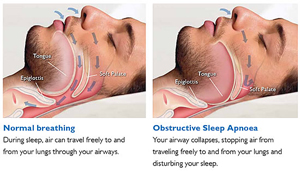 Produced during sleep, snoring is the sound created by typical vibrations of structures in the throat. While snoring can have important effects, it can also be a sign of serious problems like obstructive sleep apnea. There are several types of sleep apnea, but the most common is obstructive sleep apnea. This type of apnea occurs when your throat muscles intermittently relax and block your airway during sleep. This results in a drop in oxygen levels.
Produced during sleep, snoring is the sound created by typical vibrations of structures in the throat. While snoring can have important effects, it can also be a sign of serious problems like obstructive sleep apnea. There are several types of sleep apnea, but the most common is obstructive sleep apnea. This type of apnea occurs when your throat muscles intermittently relax and block your airway during sleep. This results in a drop in oxygen levels.